Vomiting Golden
10-year-old MN Golden Retriever
The patient initially presented to a local ER with a history of weight loss and chronic intermittent vomiting over the prior few weeks. The owners reported that the stools had been soft and sometimes dark in color. The owner decided to take him to the ER when he stopped eating that weekend.
Radiographs taken at the ER showed marked gas dilation of several small intestinal segments. A circular soft tissue opacity was noted in the right caudal abdomen. A small caudal vena cava was noted, indicative of hypovolemia.
Due to concern for mechanical obstruction, surgical exploration was recommended. The patient was treated symptomatically with SQ fluids and Cerenia, taken home overnight and re-presented at a general practice the following morning.
QAR. BCS 2/5. Temp 102.7. The patient was moderately dehydrated and painful on abdominal palpation. On a rectal exam, dry dark stool was noted. The remainder of his exam was non-remarkable.
CBC: mild lymphopenia 0.63 K/uL (normal 1.06-4.95K/uL)
Chem: WNL
Unable to obtain urine for a UA
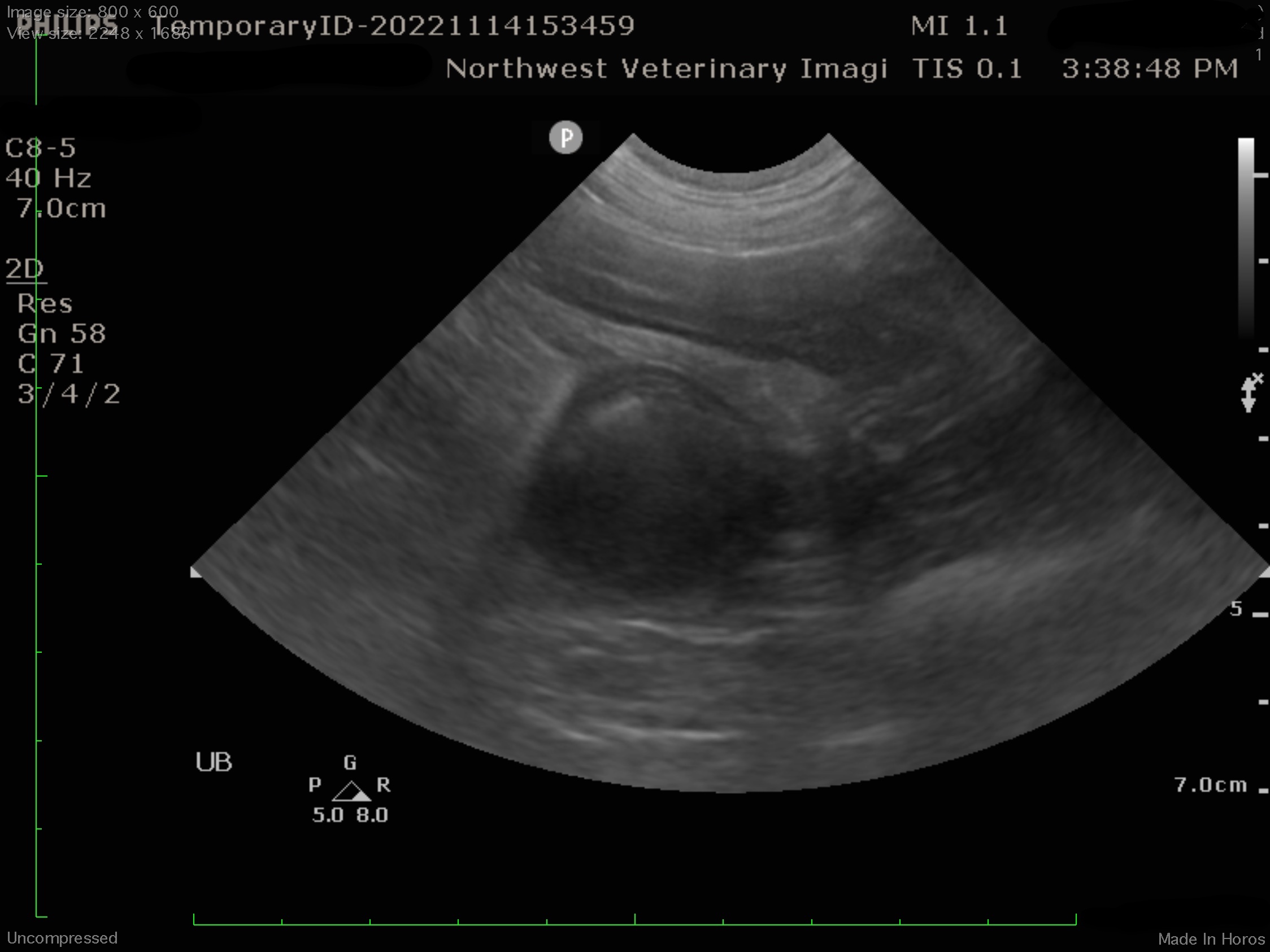
Radiographs were repeated to confirm the presence of the suspected foreign material. While an obstruction was suspected, no foreign material could be visualized. Our mobile radiologist performed an urgent abdominal ultrasound at the referral practice to further characterize the abdominal pathology prior to taking the patient to surgery.
Jejunal mass and intussception
Ultrasound findings: There is an approximately 10 cm length jejunal intussusception. There is impression of a 2cm diameter solid hypoechoic mass associated with one end of the intussusception. The muscularis and submucosal layers of small intestines appear diffusely thickened.
Treatment Plan: The patient was taken to surgery. At surgery, an intussusception of the jejunum was found. Once the intussusception was reduced, a 2cm, solid, round intra-luminal mass extending on a stalk from the mucosa was identified. A resection and anastomosis was performed. Biopsies were obtained of the aboral and adoral small intestine. All tissues were submitted for histopathology evaluation.
Histopathology Results:
1. Jejunum (with mass): Leiomyoma, completely excised
2. Proximal jejunum: Mild lymphoplasmacytic and eosinophilic enteritis with mild neutrophilic serositis
3. Distal jejunum: Minimal lymphoplasmacytic and eosinophilic enteritis
Case Outcome: The patient recovered well from surgery and no further intervention was recommended.
Discussion: Leiomyoma is typically a benign neoplasm originating from the smooth muscle wall of the GI tract. Masses are typically discreet and solitary. Surgery is the treatment of choice and is often curative. Leiomyosarcoma, on the other hand, is typically invasive and metastasis can be seen in ~30% of cases. Tumors can also recur locally after an incomplete, or even an apparent complete excision. Median survival after surgery ~1 year. Chemotherapy results are anecdotal.